More Specialist Toolkits
Mutational Toolkit | Questions Toolkit
Dear fellow patient,
A cholangiocarcinoma (CCA) diagnosis can be overwhelming, but you are not alone. Our toolkit is designed to help guide you forward with the gift of knowledge, experience, and wisdom from fellow patients and caregivers who have been in your shoes.
Bridging the Cancer Information Abyss
The CCA Toolkit app provides a roadmap and a bridge to a pathway traveled by other cholangiocarcinoma patients. Our goal is to better equip and empower your capacity to mount an effective and robust response to your diagnosis.
Ultimately you are the captain of your own ship, and you need to lead this challenge – others will follow your lead. Be open-minded, be willing, be consistent, and trust yourself.
Steve Holmes
Fellow Patient
A Gold Standard Knowledge Pathway to better decision making
Being an informed patient means you understand the information in a way that you can proactively act on it to make better quality decisions. This is the first crucial step towards becoming an “Empowered Patient.”
Think of the content below, as sequential stepping stones of knowledge. Understanding this sequence will greatly improve your understanding and provide a significant advantage in your interactions with medical professionals and subsequent decision-making.
- DNA: We are all individually uniquely DNA coded. This makes us who we are.
- DNA Replication: Our DNA is constantly making copies of itself.
- Replication mistakes in copying DNA often happen due to things like sun exposure, smoking, what you eat, and even stress.
- DNA Spell Checker: Think of your immune system as a DNA spell-checker, fixing errors and getting rid of cells that can’t be fixed.
- Unrepaired Mistakes: When the Immune system misses or is unable to repair a DNA mistake, the cell becomes mutated (bad rogue cells) and will continue to grow and multiply unchecked.
- Mutations: These rogue cells can become tumors, and some may turn into cancer.
- New technology can spot these DNA errors through special tests like immunohistochemical (IHC) analysis and molecular profiling.
- IHC (Immunohistochemistry) is a quick lab test using special dyes to find abnormal proteins (Biomarkers) in tissue samples.
- Molecular profiling dives deeper into the tissue sample, looking at the tumour’s genetic makeup to find what might be causing the cancer.
- Tissue samples These samples are usually taken during surgery or a biopsy. If that’s not possible, blood tests are another option. increasingly, it can also provide ctDNA information (ct = circulating tumour) which is tumour shedding material in the blood.
- ctDNA: “Blood tests look for ctDNA, which is basically pieces of the tumor floating in your blood.”
- Pharmaceutical: Drug companies are always working on treatments that target these specific mutations.
- Immune support: This treatment boosts and supports your immune system to help it spot, target, and eliminate cancer cells it has missed or has managed to evade detection.
A Pathway to Inner Strength and Resilience
Attitude is an essential ally in combating cancer. The following insights are distilled from observations of patient success, serving as an inspirational guide.
Understanding this sequence can empower you to better navigate the unique challenges of cancer:
- Our Values stimulate our innermost willingness and visions
- Willingness drives our visions
- Vision shines a light on our direction
- Direction stimulates our purpose
- Purpose generates our inner momentum
- Inner Momentum is our first unseen momentum, it unlocks and opens us up to new thoughts
- Thoughts are things that are sensory data input from our environment, that stimulate our thinking and actions
- Thinking is the action that activates or acts on our thoughts, shaping and refining our momentum and attitude
- Attitude is the sum of our thoughts and actions, shaped by our values.
Remember, if our values form the foundations of our attitudes, conflicts in our values will/can impact our overall attitude. Keeping an attitude aligned with our values helps empower our capacity to rise above the many challenges. This alignment can make distinct differences as we move through and beyond the diagnosis.
Understanding and choosing the right caregiver is an important decision that can make a significant difference in your cancer journey. The contents of this section should be discussed and understood by you both.
What you need to know
Your caregiver should be a person who knows you well and is able to get alongside you, a person who can willingly provide assistance and support to cover your limitations both physically and emotionally.
Why do you need to know
Your caregiver will help you with your daily activities and ensure that you remain on track for your objectives.
Together you will both evolve into a team, this does take and requires pause, poise and consistency by you both.
Please remember that your caregiver will also need good support to be the best they can be.
Important note
Choosing the right caregiver isn’t just about who’s around. You both need to vibe—especially under the emotional weight of a cholangiocarcinoma diagnosis. It’s easy to just react instead of planning. Take a moment to get on the same page. Your roles will likely differ, and that’s okay. If you’re scouting for a caregiver from scratch, pick someone you can trust, someone who’s got the qualities you need.
Attributes of a Good Caregiver
Your caregiver needs to acquire specific skill sets, and often this is more about knowing what they are and fine-tuning as you go. But you also need to elevate your own game and rise above your best. When you’re at your best, it brings out the best in those around you, and this is vital in overcoming cholangiocarcinoma
- Good Listener: Must listen well, have no judgments, and understand your needs and concerns.
- Open & Willing: They’re your go-to for real open-minded talk, asking questions and allowing you to feel comfortable in speaking your mind and expressing your innermost thoughts and feelings. They build a supportive environment around you both.
- Team Builder: They’re your team builder and connection hub, linking you with doctors, family, and friends who can help.
- Manager: Reducing chaos and overwhelm by sorting—appointments, information, and emotions—so you don’t have to.
- Decision Maker: Your caregiver will help you organise questions, simplify choices, and build a strong foundation for decision-making. They help you with the information needed to make informed decisions.
- Advocate: They’re your voice when you can’t find your own or are unable to say it as you would like.
When it comes to cholangiocarcinoma and surgery, it’s all about understanding your options. Surgery can be a potentially curative treatment, but it depends on where the tumour is located.
What you need to know
- Liver resection: This involves removing part of the liver where the tumor is located.
- Whipple procedure: This surgery is more extensive and involves removing a portion of the pancreas, small intestine, and bile duct in addition to the affected part of the liver.
- A combination of both: Sometimes, a combination of liver resection and Whipple procedure may be necessary depending on the tumor’s location.
- Potentially a liver transplant: In some cases, a liver transplant may be an option, especially if the cancer has not spread beyond the liver.
Why do you need to know
It’s crucial to know these options because it helps you research and understand what might work best for your specific case.
Important note
Now, here’s an important note: If surgery is a possibility but seems too risky due to the tumor’s location or size in relation to other vital organs, neoadjuvant chemo, targeted therapies, or radiation treatment may be used to shrink the tumor before attempting surgery. Seeking second and third opinions is common before making a final decision.
In summary, surgery is the primary curative option for cholangiocarcinoma, and neoadjuvant therapy followed by surgery is considered the next best option. Both have their risks, so it’s wise to seek multiple opinions to make an informed choice. The second option does carry the added risk of metastases occuring during the neoadjuvant period, which could prevent surgery. It’s a complex decision, but having all the information is key.
Attributes of a Good Surgeon
When you’re looking for a surgeon to tackle cholangiocarcinoma, there are some key attributes you should consider:
- Specialisation: First and foremost, you want a surgeon who knows and specialises in cholangiocarcinoma or has current experience with a very similar GI liver and pancreatic condition. Their expertise in this area is crucial for seeking accurate advice and guidance.
- Expertise & Experience: It’s not just about expertise but also about their experience. Seek a surgeon who preferably has current experience with your exact diagnosis or similar to yours. This hands-on knowledge is invaluable.
- Second Opinion: Your surgeon should be totally fine with you seeking a second opinion. Second opinions can be lifesavers and are a standard part of the decision-making process in complex medical cases.
- Updated Knowledge: Medicine is always evolving. Your surgeon should be up-to-date with the latest treatments for cholangiocarcinoma, including knowledge of ongoing clinical trials. This shows their commitment to staying informed about the latest research and technological advancements.
- Communicator: A good surgeon should also be a good communicator. They should be open to discussing your questions, observations, and opinions. It’s your health, and you should feel comfortable discussing it with your medical team.
The Oncologist is the captain of your ship:
Choose an oncologist who not only knows about Cholangiocarcinoma but has current expertise and experience in treating it. Preferably, they should be actively treating patients. An experienced oncologist in cholangiocarcinoma will go the distance with you, serving not just as a short-term guide but as a committed partner who will see it through.
What you need to know
Your oncologist’s expertise and experience, communication skills, and openness to clinical trials and second opinions are all important factors in choosing the right oncologist for your specific diagnosis.
Why do you need to know
Specific expertise can mean the difference between life and death when it comes to treating serious cancer. Good communication and access to clinical trials and second opinions can also greatly impact treatment outcomes.
Important notes
- Don’t allow yourself to become just a number.
- Do not get trapped with a well-intentioned Oncologist who clearly does not have the expertise or experience – this is a common mistake and a strong reason to seek an independent second or third opinion.
- Choose an oncologist who is willing to listen to your observations, suggestions, and questions.
- When it comes to treating a serious cancer, specific expertise, experience, and attitude can mean the difference between life and death.
Attributes of a Good Oncologist
- A Good Captain: You and your Oncologist must establish a solid trusting relationship – you must be comfortable with your choice.
- Specialization + Experience: Your oncologist should have a history of treating Cholangiocarcinoma patients, ensuring they can provide accurate advice, guidance, and effective treatment options.
- Biomarkers Matter: Your oncologist must be fully conversant and familiar with Cholangiocarcinoma biomarkers and mutations.
- IHC Testing: Ensure your Oncologist provides your IHC test results. Ask for a copy for your personal file.
- NGS Molecular (Genomic) Profiling: If an IHC test does not provide a match to current targeted or immunotherapy clinical trials, ask your Oncologist to order a molecular profiling of the tumor tissue.
- Clinical Trials: The oncologist should be actively involved with clinical trials related to Cholangiocarcinoma.
- Second Opinions: Your oncologist should be comfortable and supportive of you seeking a second opinion, as second opinions often play a critical role in treatment decisions.
Selecting the right hospital is a critical decision for cancer patients. Often, the best hospitals are associated with top-notch surgeons, oncologists, and supporting professionals. It requires thorough research and careful consideration, tailored to your specific diagnosis. It is more than worth the effort. If you begin in a hospital due to circumstances you can still make the necessary change.
What you need to know
In making this crucial decision, consider the following key factors:
- Expertise of medical professionals in the hospital
- Available * ‘Upper GI’ resources and treatment options
- Location and accessibility
- Reputation and patient satisfaction rates
*Upper GI; Upper Gastrointestinal
Why do you need to know
Your hospital choice can profoundly influence your care. Hospitals with greater resources and expertise typically achieve better treatment outcomes and higher patient satisfaction rates. Additionally, they may provide greater access to clinical trials featuring innovative therapies.
Important note
When making your hospital selection, start by discussing your options with your GP or primary care physician. They can offer recommendations or refer you to specialists and hospitals that align with your needs.
If you find yourself in a remote area, consider hospitals that are open to collaborating with a larger hospital or oncologist in a city.
Attributes of a Good Hospital
- Location: Hospitals in major cities or top regional centres usually have cutting-edge technology and top-notch professionals.
- Cancer-Specific Hospital: Specialised hospitals often offer better diagnostic and treatment options specifically tailored for cancer.
- Medical Expertise: Seek hospitals where the staff has a strong track record in treating cholangiocarcinoma.
- Clinical trials: Some hospitals offer and specialise in ‘Upper GI’ Cancer, providing easier access to innovative treatments still in the research phase. Keep an eye out for these, as they can offer more potentially lifesaving options.
- Reputation: Check hospital ratings, patient reviews, and satisfaction to gauge the quality of care. Don’t hesitate to ask your GP and local nursing staff for recommendations. You can also seek advice from members of the Cholangiocarcinoma Australia Community Facebook Group.
The exact location of the primary tumour determines the subtype of Cholangiocarcinoma and the appropriate treatment pathway.
What you need to know
- Tumor Location: Understand where your first tumour began, this is known as your primary tumour
- The primary determines the exact subtype of cholangiocarcinoma and the diagnosis
- Can it be surgically removed? or has it metastasised (Spread)
- If it cannot be removed can a surgeon obtain a biopsy from it ((tissue sample)
- If it cannot be surgically removed can neoadjuvant therapy become an option
Why do you need to know
- Primary Locations determine treatment approaches
- Surgical Potential: If the primary tumor remains localised, this provides surgeons with the opportunity to remove all of the tumour
- If surgery is not an option, then ask if neoadjuvant treatment can shrink the tumor for surgery
- Seek second and third opinions before accepting that surgery is not an option – this approach also apply’s to obtaining a biopsy
- Biopsy: A Biopsy provides valuable insights into the tumour’s genetic makeup, aiding in a deeper understanding of its growth drivers and potential targeted and clinical trial treatment options. Refer to IHC testing and Molecular Profiling
Important notes
- Consult with experienced Cholangiocarcinoma surgeons and Oncologists to ensure you receive the best advice.
- Seek Second opinions only from proven experts in Cholangiocarcinoma
- Biopsy: Ask for an IHC Test and then Molecular (Genomic Profiling)
Sub-types of Cholangiocarcinoma
The location of the first tumour (Primary) determines the subtype, it is important that you understand this.
- Intrahepatic: Refers to a primary tumour that originates in the bile duct within the liver. (Learn More)
- Extrahepatic – Perihilar: Refers to a primary tumour that originates in the bile duct at the junction where the bile ducts join just outside the liver. (Learn More)
- Extrahepatic – Distal: Refers to a primary tumour that originates in the bile duct outside the liver region further down the common bile duct near the pancreas. (Learn More)
Associated Bile Duct Cancers
- Gallbladder Cholangiocarcinoma: A primary tumor originating in the gallbladder, affecting its bile ducts, leading to cancerous growth. This form of cancer is relatively rare.
- Ampullary Cholangiocarcinoma: This Cholangiocarcinoma type originates in the ampulla of Vater, a small structure where the common bile duct and pancreatic duct join, leading to cancerous growth. It is also relatively rare.
Which are you?
Intrahepatic Extrahepatic – Perihilar Extrahepatic – Distal Gallbladder AmpullarUse the printable diagrams below to help or use the Patient Navigator Journals with your Doctor.
Must Do Checklist
What is your subtype? Can it be surgically removed? If not nan it be biopsied? If not can neoadjuvant treatment be used to shrink the tumour? Does your Medical Professional have current expertise and experience in your cholangiocarcinoma? Discuss obtaining a neutral second opinion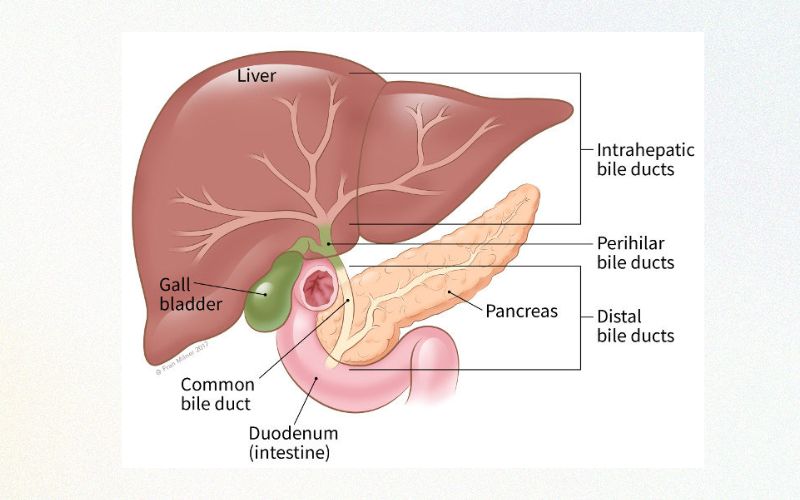
Understanding the stage of your cancer is a vital step in gaining a comprehensive understanding of your current condition. This process not only aids your medical team but also empowers you with valuable insights into navigating and measuring your journey effectively.
What you need to know
Determine whether the primary tumor remains stable and localised, if it has invaded the walls of the bile duct, or if it has spread to other locations (metastasis).
Staging the cancer provides critical information that directly influences your treatment options.
Why do you need to know
Comprehending the stage of your cancer empowers you to make informed decisions, communicate effectively with your doctor, and explore all available treatment options, including the potential for a complete and potentially curative surgical removal. It also instills a sense of control and confidence, enabling you to actively understand and participate in your treatment decisions.
Important note
Second and/or third opinions are vital at this point, so do not be afraid to ask for them. Second opinions should be unrelated to each other.Staging Attributes
Know your stage: Provides essential information about the extent and spread of cancer in the body. Predicting: It is an essential tool for predicting the prognosis and determining the appropriate treatment plan. Informed Decisions: Staging allows doctors to compare the outcomes of different treatment options and make informed decisions. The TNM system: Is the most common system used for cancer staging.
HC (Immuno-histo-chemistry) is a rapid chemical staining test on tissue samples. This test is typically completed locally within 5 days, using tissue obtained from your surgery or a biopsy. Its purpose is to identify proteins found (expressed) on the surface of our cells, known as biomarkers. This provides evidence of the cell’s activity and can reveal known DNA mutations (mistakes) that are associated with certain types of cancerous tumours
What you need to know
Biomarkers are like clues about your cancer’s specific type, stage, and behaviour. They can also reveal genetic mutations that might be driving the cancer’s growth.
Why do you need to know
Knowing which biomarkers are present in your cancer can guide your medical team toward the most effective treatments, including cutting-edge immunotherapies. For example, if your IHC results show biomarkers like PD-L1, MSI-high, CTLA-4, HER2, or dMMR, you might be eligible for certain clinical trials targeting these exact features.
Important notes about these biomarkers
- T-cells act like our body’s security team.
- They have checkpoints on their surface, like CTLA-4 to prevent excessive activation of T-cells, also the y have PD-1
- PD-1 scans for PD-L1 on cell surfaces
- Healthy cells express PD-L1 to approaching T-Cells. When PD-L1 binds with PD-1 it deactivates the T-Cell attack
- This binding is known as “The Checkpoint Pathway”
- Cancer Cells can sometimes evade activated T-cells by expressing PD-L1 and deceiving the T-cell
- Immunotherapy drugs have been developed to block this pathway and binding to allow the T-cell to see and attack
*As a newly diagnosed patient, you must be aware of your biopsy’s biomarkers result. Is it a match for (ICI) “Immune Checkpoint Inhibitor” treatment? This is something you should know before committing to a treatment plan. If an IHC test is not helpful ask your oncologist to order a Genomic (Molecular) Profiling as your next option.
IHC Immuno-Histo-Chemical
- “Immuno-“ refers to the immune system and the use of components of the immune system, which includes antibodies that are used to recognize and bind to specific antigens (proteins) in the tissue.
- “Histo-“ comes from the Greek word “histos” meaning tissue. So, in this context, it refers to the study of biological tissues.
- “Chemistry” relates to the chemical reactions that occur when the antibodies bind to the antigens and the subsequent reactions that produce a visible signal, often a color change, which can be seen under a microscope.
So, Immunohistochemistry is a process that uses antibodies to detect specific antigens in tissues, and this detection is visualized through a chemical reaction that produces a color change. It’s like a highly specific and targeted coloring book where the antibodies are the markers that only color certain patterns (antigens) in the tissue. This allows doctors and scientists to see the presence and location of these antigens, which can be crucial for diagnosing diseases, including cancer.
IHC Attributes
Chemical Staining: IHC testing uses chemicals to identify specific biomarkers associated with different tumor types. Fast & Efficient: It quickly determines the presence of essential biomarkers, guiding treatment options. Relevance: Biomarkers such as PD-L1, MSi-high, dMMR, HER2, and CTLA-4 match clinical trials and targeted treatments. Biomarkers: CTLA-4 and HER2 Identifying: IHC results identify cancer type, stage, grade, and mutations driving tumor growth.” dMMR; deficient mismatch repair. MMR is responsible for correcting mistakes in DNA replication. MMR is made up of four genes that monitor and correct mistakes as they occur (much like a spell checker), when one or two of these genes stop working, mistakes can go unrepaired, MMR is now described as “d’ for deficient. dMMR can lead to microsatellite instability (MSI). If one gene is silent this translates to MSi-Low if two or more are silent this translates to MSi-high. ICI – immune Checkpoint Inhibitors have shown favourable responses to this combination.Further Notes:
Your Priority Checklist
What is your PD-L1 Score
What is your MSi Status
What is your MMR status – is it deficient? (dMMR)
Is CTLA-4 present
Is HER2 present
Genomic Profiling: A Roadmap for Personalised Treatments
Genomic profiling is a game-changer in cancer. If your IHC test doesn’t reveal suitable biomarkers for clinical trials, request Next Generation Sequencing (NGS), also known as Genomic or Molecular Profiling.
What you need to know
Biomarkers Matter- Genomic profiling identifies the genetic mistakes and mutations driving the growth of a tumor, and potential clinical trial treatments.
- Without a molecular profile, your oncologist can only use chemotherapy and radiation treatments, unaware of the underlying drivers of your cancer.
- Be prepared to wait 4-6 weeks for results.
- Blood biopsy can be used if tissue is not available.
Tumour Samples Types:
- Tissue from Surgery
- Tissue from a biopsy procedure,
- Blood Biopsy Option: Just know it’s not as spot-on as a tissue test.
This test also known as liquid biopsy, tests bits of material — like molecules or whole cells — that your tumor sheds into the blood, urine, or other body fluids. For some cancers, liquid biopsies can be used today to test for some of the same molecular features of cancer as tissue biopsies.
Why do you need to know
- Cholangiocarcinoma frequently presents actionable mutations, making genomic profiling vital. These mutations can be specifically targeted with immunotherapies.
- Identifying these mutations through profiling empowers your oncologist to create a personalised treatment plan aimed at eradicating the cancer.
Important notes
- Targeted immunotherapy, which identifies and attacks specific mutations driving cancer growth, is the future of cancer treatment.
- An oncologist with expertise in genomic profiling results and their relevance to ongoing clinical trials and treatment options is crucial.
- Biomarkers like PD-L1 expression, MSi, and TMB status can predict your response to immunotherapy and checkpoint inhibitor therapy, offering potential life-saving opportunities.
- Other relevant Biomarkers: CTLA-4 and HER2
Molecular/Genomic Profiling Attributes
- High rate of Actionable Mutations: Specific mutations can be targeted with available therapies.
- More effective treatment: Personalised treatments target the precise genomic alterations driving your cancer.
- Improved prognosis: Precision medicine improves overall prognosis and survival rates.
- Better response to treatment: Identifying specific genomic alterations helps identify potential treatment resistance.
- Clinical trial participation: Profiling can match you with ongoing clinical trials for potential life-saving treatments.
Further Explanation
In genetic studies, researchers examine an individual’s entire set of genes to identify inherited mutations or risk factors. In genomic studies, the focus is on the genes within cancer cells to pinpoint mutations driving cancer growth and determine the best treatment based on the tumour’s molecular profile.
In contrast, in genomic studies, scientists are focusing specifically on the genes in the cancer cells to identify mutations or alterations that are driving the cancer’s growth and to determine the best course of treatment based on the tumour’s molecular profile.
For more details click here
Your Priority Checklist
Order a Genomic Profile Highlight PD-L1 / MSi Status Highlight MMR status Highlight TMB Status Keep a copy of results on fileAfter diagnosing and staging cholangiocarcinoma, your doctor will discuss treatment options with you.
What you need to know
- Surgery is considered the sole potentially curative option.
- First-line treatment for cholangiocarcinoma is surgery. If surgery is not feasible, neoadjuvant chemotherapy followed by surgery and adjuvant chemotherapy with Gemcitabine/Cisplatin is the next option recommended.
- For inoperable cases, Gemcitabine/Cisplatin and radiation therapy are first-line treatments. Note; at the time of writing ‘Gemcitabine/Cisplatin/Durvalumab’ is first-line in the USA.
- Second or third-line treatments may include different combinations, even immunotherapy clinical trials.
Why do you need to know
- Understanding available treatment options is critical for making informed decisions that could really help improve your outcomes.
- Each treatment approach carries unique benefits and risks, with your specific situation guiding the best choice.
- Understanding these choices means you can have better discussions about these options with your doctor. Understanding empowers your real knowledge, and helps focus your research and decision-making.
Important notes
- Identifying relevant biomarkers like PD-L1, MSi-High, and TMB-High before treatment, especially for immunotherapy, is crucial.
- Early eligibility determination for clinical trials is necessary, as prior treatments may disqualify participation. Ensure your planned treatment won’t disqualify you from future trials.
Understand your treatment options
- Before starting any treatment plan – do you have biomarkers PD-L1, MSI-High, and TMB-High.
- Surgery is the only curative option for cholangiocarcinoma.
- Chemotherapy is a treatment designed to destroy all rapidly dividing cells, healthy or cancerous.
- Gemcitabine works by interfering with the growth and spread of cancer cells in the body.
- Cisplatin works by damaging the DNA in cancer cells, which prevents them from dividing and growing.
- Radiation Therapy uses high-energy radiation, such as X-rays or protons, to kill cancer cells.
- Targeted Therapies are treatments that target certain tumour cell parts that are fuelling cancer growth.
- Immunotherapy is a biological treatment that helps your own immune system fight cancer.
Explanations
- Neoadjuvant therapy is a treatment given before surgery to shrink the tumour and/or reducing the risk of cancer spread.
- Adjuvant therapy is administered after primary cancer treatment to reduce the risk of cancer recurrence
- Ineligibility for Surgery: Can a biopsy be obtained? Seek Second Opinions to be certain.
Your Priority Checklist
Doctor has Cholangiocarcinoma Expertise & Experience Surgery Eligibility Biopsy Eligibility Neoadjuvant then Surgery PD-L1, MSi-High, TMB-High mmunotherapy EligibilityUnderstanding the role of surgery in Cholangiocarcinoma treatment is crucial. Surgery is currently the only known curative option, but it may not be feasible in all cases, particularly if the cancer has metastasised.
Types of Surgery
Surgery options for bile duct cancer vary depending on tumour location, with different options for intrahepatic, perihilar, distal, and liver transplant cases. If surgery is not an option obtain a biopsy for molecular testing.
Surgical Options
- Intrahepatic: Liver Resection Surgery is an option if the tumour is located in the bile duct within the liver. Surgeons may remove up to 75% of a patient’s liver. Full liver transplants may also be an option in some cases.
- Extrahepatic – Perihilar: This location may require a combination of liver resection and Whipple surgery.
- Extrahepatic – Distal: Whipple surgery is an option if the tumour is located in the bile duct outside the liver, specifically in the common bile duct.
- Liver transplant: Surgery may be an option for some patients.
It’s important to note that surgical options may vary depending on the surgeon’s approach, experience, and risk analysis. A second or third independent opinion is common.
Important notes
It’s important to note that surgical options may vary depending on the surgeon’s approach, experience, and risk analysis. A second or third independent opinion is common.
Choosing your Surgeon
Choosing an experienced surgeon for Cholangiocarcinoma surgery is critical for optimal outcomes. Consider communication skills and seek a second independent opinion to ensure the best care.
Summarising surgery as a treatment
- Surgery is the only known curative option for cholangiocarcinoma, but eligibility depends on the tumour’s location, size, and stage
- Different types of surgeries are available depending on where the tumour is located, including intrahepatic, perihilar, distal, and liver transplant surgeries
- Neoadjuvant chemotherapy and/or targeted radiation may be used to reduce tumour size before surgery
- The choice of surgery depends on the surgeon’s approach, experience, and risk analysis
- Choosing the right surgeon with specific expertise and experience is critical for optimal outcomes, and it is recommended to seek a second independent opinion
- After surgery ensure that an IHC test is immediately conducted, highlighting PD-L1 score, MSi and MMR status and that there is also enough tissue sample remains for NGS profiling if/when required
Explanations
- Neoadjuvant therapy is a treatment given before surgery to shrink the tumour and/or reduce the risk of cancer spread
- Adjuvant therapy is administered after surgery to reduce the risk of cancer recurrence
Your Priority Checklist
Surgeon has CCA Expertise Curative Surgery Eligibility Neoadjuvant then Surgery Liver Resection Surgery Liver Transplant Surgery Whipple Multi-Organ SurgeryAre you a candidate or could you become a candidate for a Clinical Trial? Clinical trials are an essential component in a Cholangiocarcinoma patient’s treatment toolkit. They offer access to the latest cutting-edge treatments and opportunities.
What you need to know
Clinical trials are research studies aimed at evaluating a medical intervention. They are used to learn if a new treatment is more effective and/or has less harmful side effects than the standard treatment.
What you need to know
Clinical trials offer more options and opportunities when the current first-line treatment is not working. Clinical trials also offer you the opportunity to become involved in treatments that may well become tomorrow’s standard of care.
Important notes
It is important to prioritise consulting with an Oncologist who has the expertise and experienced with Cholangiocarcinoma and clinical trial options. Do not assume that your oncologist has the necessary experience, instead, ask them directly.
- Learn more about Clinical Trials
- Find a Clinical Trial
Trial Terminologies
- ORR (Objective Response Rate): The percentage of patients given a new treatment whose tumor shrinks or disappears by a certain amount within a defined period of time.
- PFS (Progression-Free Survival): How long a person keeps living without their cancer getting worse after starting a new treatment.
- OS (Overall Survival): How long a person keeps living after starting a new treatment.
Clinical Trial Phases
- Phase 1: First in Human trial – Focuses on safety issues like side effects, dosages, and how the drug works in the body.
- Phase 2: Focuses on both safety and the drug’s effectiveness. Typically lasts several months to a few years.
- Phase 3: Focuses closely on how well the drug works in a larger, specific population group of people and any side effects. Usually takes several years to complete.
Clinical Trial Attributes
- Innovative Treatment: Trials provide you the opportunity to become part of new options not yet available in standard care.
- Hope and Opportunity: Clinical trials provide structure and purpose to your hope, through access to new treatments and the potential for better outcomes.
- Clear Objectives: Clinical trials have well-defined and clear objectives that define the purpose and scope of the study.
- Monitoring and Surveillance: Clinical trials typically have more frequent and rigorous monitoring and surveillance protocols than standard of care treatments to ensure patient safety and to collect accurate data on the effectiveness of the treatment. Many patients see this as an advantage because it provides them with more personalised care and attention.
- Costs: Most Clinical Trials cover all your related costs.
Your Priority Checklist
Trial Eligibility Doctor has CCA experience Doctor has Clinical Trial experience Ask about Future Eligibilities Phase of trial – 1 , 2, or 3Second opinions can introduce new and potentially life-saving options, especially if the “Gold Standard” is not being followed.
What you need to know
A second opinion is another medical opinion from an independent doctor other than your current doctor and who has current Cholangiocarcinoma expertise.
What you need to know
Doctors can make mistakes or have varying opinions on the best course of treatment. Some can be too conservative, not up to speed and even fatigued. Getting a second opinion from another unrelated doctor with current expertise can provide peace of mind and potentially lead to a different treatment plan or diagnosis.
Important notes
Many doctors support their patients seeking second opinions. Additionally, consider remote second opinions to access a broader range of expertise, especially if travel is challenging.
Observations
The first diagnosis isn’t always correct or complete. According to a study by the Mayo Clinic, 88% of original diagnoses were changed or refined by a second opinion.
A second opinion can provide alternative options, which can benefit the patient physically, emotionally, and financially. Even just a confirmation of a diagnosis can provide peace of mind.
Second Opinion Attributes
- Expertise: The second opinion should come from a doctor who has current expertise in Cholangiocarcinoma and is experienced in providing second opinions. It’s important to seek a second opinion from a doctor who is knowledgeable in the latest treatments and research.
- Remote Opinion: The opportunity for a remote opinion increases the choice of more experienced oncologists with current expertise.
- Independent Opinion: The second opinion should be an independent opinion from a doctor who has no financial or personal ties to your current doctor or medical institution. This ensures that the opinion is unbiased and objective.
- Thorough Evaluation: The second opinion should be a thorough evaluation of your medical history, test results, and diagnosis. The doctor should take the time to review all relevant information and provide a detailed explanation of their opinion.
- Clarity: The second opinion should be clear and easy to understand. The doctor should explain their opinion in plain language and answer any questions you may have.
- Respectful: The second opinion should be given with respect and consideration for your feelings and concerns. The doctor should listen to your questions and provide compassionate care throughout the evaluation process.
Your Priority Checklist
Expertise & Experience Consider Remote Opinion Independent Opinion Thorough Evaluation Clarity + RespectfulWhat is a second opinion
An opinion of a doctor other than the patient’s current doctor. The second doctor reviews the patient’s medical records and gives an opinion about the patient’s health problem and how it should be treated.
People make mistakes every day, and doctors are not immune to this fact. What’s more, some doctors are more conservative while others tend to be more aggressive. So their findings and recommendations can vary dramatically. For this reason, more and more patients are getting second opinions after a diagnosis. Whether your doctor recommends surgery, makes a cancer diagnosis, or identifies a rare disease, there are many benefits to getting a second opinion. These benefits include everything from peace of mind and confirmation to a new diagnosis or a different treatment plan.
Many people do this, and most doctors are comfortable with it. You can get a second (or third, or more) opinion for any reason. Some reasons people have given are: You want to know every possible choice for treatment.
For more insights and information on obtaining a second opinion visit our dedicated “Second-Opinion” page
Neoadjuvant + Adjuvant
Neoadjuvant therapy is a treatment given before surgery to shrink the tumour and/or reducing the risk of cancer spread.
Adjuvant therapy is administered after primary cancer treatment to reduce the risk of cancer recurrence.
Intrahepatic Diagnosis
These cancers are in the bile ducts within the liver. To treat these cancers, the surgeon cuts out the part of the liver containing the cancer. Removing part of the liver is called a partial hepatectomy. Sometimes this means that a whole lobe (section) of the liver must be removed, this is called a hepatic lobectomy. It is a complicated operation and requires an experienced team of surgeons and assistants. If the amount of liver tissue removed is not too great, the liver will function normally because its tissue has the ability to grow back. (Source CCF)
Extrahepatic Diagnosis
Extrahepatic Distal cholangiocarcinoma (bile duct cancer): These cancers are further down the bile duct near the pancreas and small intestine. Along with the bile duct and nearby lymph nodes, in most cases the surgeon must remove part of the pancreas and small intestine. This operation is called a Whipple procedure, this is a complex procedure that requires an experienced surgical team. (Source CCF)
Perihilar Diagnosis
These cancers begin where the branches of the bile duct first leave the liver. Surgery for these cancers requires great skill, as the operation is quite extensive. Usually, part of the liver is removed, along with the bile duct, gallbladder, nearby lymph nodes, and sometimes part of the pancreas and small intestine. Then the surgeon connects the remaining ducts to the small intestine. This is not an easy operation for the patient, and there can be surgical complications. (Source CCF)
More Toolkit Resources
Know what questions to ask medical professionals
Simplifying and demystifying to increase your understanding
Join a Private Facebook Group
Click here for CCA Australasian a private group
You will find that specific focus groups have considerable patient and caregiver experience and are connected worldwide. Everyone begins with not knowing what they do not know, this is a very scary starting position but it is essential that you start – we all begin from this same position.Many groups are part of cancer organizations that focus on and fund research on your exact cancer. Private Facebook Groups are Private and respectful, with rules of membership. Groups are often formed separately for the patient and caregiver to ensure transparency and full engagement.
Facebook Groups are very resourceful
Facebook Groups are very resource and experience-rich and will educate you on what to read and research.
Groups and their members will help you screen out avalanches of irrelevant information that can overwhelm you.Facebook Groups provide a window on what is working today.
The medical communities information channels typically move very slowly.
Highly focused private Facebook groups share results and upcoming treatment options, they have considerable global patient and caregiver connections and experience. Think of these groups as real-time in terms of results and new options that you and your oncologist will not be aware of.NON Facebook Groups
Many cancer organization websites run their own private member-only groups, ie not a Facebook Group. Please be aware that these types of groups can be less worldly and more insular in their shared knowledge.
Become Open and Willing to Communication
It is very important to create a communication foundation that allows you to express yourself as yourself, this will help you learn and move forward more efficiently.
The medical community’s terms, terminologies, phrases, language, and descriptions are not always in sync. Different names and terms are used by different countries and cohorts. This becomes confusing to the patient and caregiver, we try our best to overcome this.
This is not a complete list, but it will get you started in the right direction.
NCI Directory of Medical Terms
Advocate
People who can speak up, advance the patient and caregiver questions, and generally support the effort. Often patients and their Caregivers have several advocates who have different skills
Adjuvant therapy
This is a treatment administered after primary cancer treatment (surgery) to reduce the risk of cancer recurrence.
Neoadjuvant therapy
Chemotherapy or radiation treatment (or a combination of both) is often given before surgery, in order to shrink the tumour or make it easier to remove. This can help to reduce the risk of cancer spread or make surgery options more feasible. It is often used for tumours that are difficult to remove or in cases where the tumour is in a sensitive location.
APC
Antigen Presenting Cells: The immunes messengers.
Antigen-presenting cells (APCs) are immune cells that process and present antigens (foreign substances) to T cells, which are another type of immune cell. This presentation of antigens by APCs is a key step in the activation of T cells and the initiation of an immune response.
B Cells
B Cells have 2 primary functions (1) Produce the ‘antibodies’ and (2) Produce memory cells for any future threats.
Biomarkers
A biological molecule found in blood, other body fluids, or tissues that is a sign of a normal or abnormal process, or of a condition or disease. A biomarker may be used to see how well the body responds to a treatment for a disease or condition.
Biopsy
This is a tissue sample that is obtained from the actual tumor.
Caregiver
The person who helps you function on an everyday basis
Clinical Trial
Clinical trials are a type of research that studies new tests and treatments and evaluates their effects on human health outcomes.
CTLA-4
A Check Point protein that sits on the surface of the T Cells. They prevent mistaken attacks on healthy cells.
CTLA-4 overview
So, the immune system is a complex network of cells that helps protect our bodies from infections and diseases. One type of cell in the immune system is called a T cell, which helps identify and attack abnormal cells, such as cancer cells.
However, cancer cells can sometimes use certain proteins on their surface to hide from T cells and avoid being attacked. This can allow the cancer to grow and spread throughout the body.
Scientists have discovered some proteins that act as checkpoints in the immune system, helping to regulate T cell activity and prevent them from attacking healthy cells. However, cancer cells can sometimes hijack these checkpoints to evade detection by the immune system.
One of these checkpoint proteins is called CTLA-4. It sits on the surface of T cells and helps prevent the immune system from attacking healthy cells by binding to proteins on the surface of other immune cells called APCs.
In cancer, some tumors can take advantage of this checkpoint and use it to avoid being detected by the immune system. But there are now treatments called checkpoint inhibitors that can block the CTLA-4 checkpoint, helping to reactivate the immune system and allowing it to attack cancer cells.
So, in simpler terms, CTLA-4 is a protein that helps regulate the immune system, but sometimes cancer cells can use it to avoid detection. However, there are treatments available that can block this protein and help the immune system attack the cancer.
So how does the tumour hijack this?
While CTLA-4 is located on the surface of T cells, some tumors can manipulate their microenvironment to increase the expression of CTLA-4 and other immune checkpoint proteins. This means some tumours are able to create an environment that stimulates more CTLA-4 expression on the T-Cells surface thus reducing the ability of the APC Cells to deliver their message. This can lead to T cell dysfunction and exhaustion, allowing the tumor to evade immune detection and destruction.
In other words, the tumor can use the body’s natural immune checkpoint mechanisms to its advantage, inhibiting the immune system and promoting its own survival. This is why targeting immune checkpoint pathways like CTLA-4 with immunotherapies such as checkpoint inhibitors can be effective in reactivating the immune response against cancer cells.
James Allison and Tasuku Honjo have jointly received the 2018 Nobel Prize in Physiology or medicine for their work on immune checkpoints. Allison and Honjo set the stage in the 1990s for the current immuno-oncology boom by discovering the cancer-killing potential of CTLA-4 and PD-1, respectively… continue reading the article
Car T-Cells
A new innovative immunotherapy technique
Checkpoint Pathway
A checkpoint pathway is a regulatory mechanism in the immune system that helps to maintain immune homeostasis (Balance / Equilibrium) and prevent autoimmune reactions.
The PD-1/PD-L1 pathway is an example of a checkpoint pathway that plays a critical role in regulating the immune response. When the PD-L1 ligand binds with the PD1 protein receptor on an activated T-Cells surface, this creates a signaling pathway to downregulate (stop) an immune attack.
Some cancers including cholangiocarcinomas can hijack this pathway to evade immune detection and attack, but immunotherapies such as checkpoint inhibitors can help reactivate the immune response against cancer cells by blocking the PD-1/PD-L1 interaction.
The percentage of cholangiocarcinomas that overexpress PD-L1 can vary depending on the study and the population being studied. In general, studies have reported PD-L1 expression in approximately 30-70% of intrahepatic cholangiocarcinomas and 50-70% of extrahepatic cholangiocarcinomas. It’s worth noting that not all patients with PD-L1 expression will respond to checkpoint inhibitor immunotherapy, and other factors such as tumor mutational burden and microsatellite instability may also play a role in predicting response to treatment.
Checkpoint Inhibitors (ICI’s)
This is an immunotherapy drug – a monoclonal antibody designed in a laboratory that interferes with the T-Cell’s “Checkpoint Switch” by locking in the “On” position, so the T Cell can continue and illuminate the cancerous tumor.
Genetic
Genetics is a term that refers to the study of genes and their roles in inheritance – in other words, the way that certain traits or conditions are passed down from one generation to another. Genetics involves scientific studies of genes and their effects. Genes (units of heredity) carry the instructions for making proteins, which direct the activities of cells and functions of the body. Examples of genetic or inherited disorders include cystic fibrosis
Genomic
Genomics is a more recent term that describes the study of all of a person’s genes (the genome), including interactions of those genes with each other and with the person’s environment. Genomics includes the scientific study of complex diseases such as cancer because these diseases are typically caused more by a combination of genetic and environmental factors than by individual genes. Genomics is offering new possibilities for therapies and treatments for some complex diseases, as well as new diagnostic methods.
IHC
Immunohistochemical is a test that uses selected chemicals to stain the tissue obtained from the tumour during surgery or a biopsy procedure. Using different chemicals creates different colour reactions to known biomarkers. In Cholangiocarcinoma samples they are looking for a response that indicates a positive response to PD-L1, MSi-high DMMR, and HER2. These biomarkers indicate potentially favourable responses to Immunotherapy treatments and or clinical trials.
Immune Checkpoints
The Immune Systems killer T-Cell has a failsafe switch to turn off any accidental attack on a healthy cell. Cancer has learned how to turn off this switch and continue growing.
Immune Checkpoint Inhibitors (ICI’s)
This is an immunotherapy drug – a monoclonal antibody designed in a laboratory that interferes with the T-Cell’s “Checkpoint Switch” by locking in the “On” position, so the T Cell can continue and illuminate the cancerous tumor.
Immune Checkpoint pathway
The Immune Checkpoint pathway refers to the interaction between the killer T-Cells and the surface of a normal cell. The T Cell has a PD-1 ligand on its surface and a healthy cell has a PD-L1 ligand on its surface (a matching pair), when these two meet and interact it turns off the unwanted T Cell attack – Cancer has learned to hide behind this by expressing PD-L1 when a T Cell approaches.
Immunotherapy
Think of immunotherapy drugs as specially designed actions that interfere with what is driving the tumor growth. A lot like a computer has code that goes wrong and a new “patch’ or string of code has to be added as a workaround. Immunotherapy is being referred to as the first-ever cancer cure – a modern-day penicillin moment in history.
HER2
Is a growth receptor gene often found on the surface of breast cancer cells – too many receptors cause cells to grow and divide too quickly, Immunotherapy treatments have shown positive results in blocking this growth pathway.
Keytruda
Pembrolizumab
Keytruda is a monoclonal antibody created in a laboratory and infused into the patient. Keytruda is not a chemotherapy treatment.
Ligand
Ligands play a crucial role in regulating immune cell function and can be targeted by using immunotherapies to either activate or inhibit the immune response.
A ligand is a type of molecule on the surface of a cell, that binds to a receptor protein on the surface of immune cells. This binding triggers a downstream signaling pathway that ultimately affects the function of the immune cell.
Using the checkpoint pathway as a relevant example: PD-L1 is a ligand and PD-1 is a protein receptor.
Tumor immune evasion.
Tumor cells are sometimes able to express PD-L1 on their surface and this can lead to them binding with PD-1 receptor molecules on the surface of an activated T-Cell. This binding triggers a downstream signaling pathway that downregulates (stops) the immune attack.
It should be noted that T-Cells are the focus of the “Checkpoint Pathway” example, but they are not the only immune cells that can be triggered by the PD-L1 ligand. Immune cells such as dendritic cells and macrophages are also involved in presenting antigens and activating T cells.
MSI
Is a measure of Microsatellite Instability
MSI-LOW
Is a low-recorded measure of Microsatellite Instability.
MSI-HIGH
Is a highly recorded measure of Microsatellite Instability.
MSS
Is Microsatellite Stable, which means no instability is present
MMR
MMR is made up of 4 proteins (MLH1, MSH2, MSH6, & PMS2 )
Mismatch Repair is the DNA repair pathway that plays a key role in maintaining our genomic stability. MMR is our “Spell Checker” correcting any errors in our DNA replication process as they occur.
dMMR
Deficient Mismatch Repair means that one or more of the 4 MMR proteins are absent and as a result, the MMR is not functioning correctly and is described as deficient. Think of dMMR as our body’s DNA Spell Checker that has become broken and as such is not able to repair DNA replication mistakes, thus mistakes continue to replicate unchecked.
Molecular Profiling
Molecular profiling provides a DNA roadmap of the tumor’s genomic and genetic environment. Genomic changes occur after birth, while genetic changes are inherited.
Molecular profiling, also known as genomic profiling, is a diagnostic tool that provides a detailed analysis of the DNA in a tumor. By analyzing the genetic material of the tumor, molecular profiling can help identify mutations and other genetic alterations that may be driving the cancer’s growth. This information can be used to identify and target the exact genetic mistakes causing the cancers growth and guide treatment decisions and select targeted therapies that are tailored to the unique genetic makeup of the tumor. Additionally, molecular profiling can also reveal information about an individual’s inherited genetic makeup, which may impact their risk of developing cancer or inform their treatment plan. Overall, molecular profiling is an important tool in the personalized approach to cancer care.
Monoclonal
Simply this is an antibody designed in the laboratory to perform one single function/purpose.
Monoclonal Antibodies
Monoclonal – means antibodies that have been designed to perform a single purpose or task.
Monoclonal antibodies are made in a laboratory and are used to block the activity of abnormal proteins detected on infected cells. They are often designed to attach themselves to protein receptors on the surface of cells infected by viruses, essentially acting as a broadcasting beacon /marker that alerts our immune system to attack.
Monoclonal antibodies have also been developed to be used as immunotherapy and help turn the immune system against a cancerous cell. For example, some monoclonal antibodies mark cancer cells so that the immune system will better recognize and destroy them, while others such as Keytruda act as a blocking mechanism.
Microsatellites
Microsatellites are stretches of DNA that contain a repetitive sequence of nucleotides
Mutations
Mutations occur when mistakes in the DNA sequence are not repaired properly, and these errors are passed on to subsequent cell divisions. These mutations can result in cells dividing in an uncontrolled manner, leading to the formation of tumors. Some tumors can become cancerous and spread to other parts of the body.
Nucleotides
Nucleotides are the repetitive strings of DNA code that make us – us. example of a code string; “AAAAA or CGCGCGCG” (codes are short tandem sequences that replicate)
PD-L1
PD1’s primary function is to switch off a T Cell attack. It does this by binding and communicating with the PD-L1 anchored to a cell surface.
PD-1 is a receptor protein that is expressed on the surface of activated T cells and interacts with a ligand called PD-L1 on the surface of other cells.
This interaction can downregulate (Stop) the activated T cell and prevent it from attacking normal cells or tissues.
In cancer, some tumor cells can overexpress PD-L1, which can prevent T-Cell engagement or lead to T-cell exhaustion. This can help the cancer to evade the immune system.
By targeting the PD-1/PD-L1 checkpoint pathway with immunotherapies such as checkpoint inhibitors (ICI), the immune response against cancer cells can be reactivated.
PD-1/ PD-L1 Pathway
Also known as the “Checkpoint pathway”
The PD-1/PD-L1 pathway is a regulatory checkpoint pathway that helps to prevent the immune system from attacking normal, healthy cells. When PD-L1, a ligand expressed on some normal and cancerous cells, binds to its receptor PD-1 on the surface of T cells, it sends a signal to downregulate (Stop) the immune response, essentially “switching off” the T cell attack. While this is important for maintaining immune tolerance and preventing autoimmune reactions, some cancers can hijack this pathway to evade immune detection and attack. By targeting this checkpoint pathway with immunotherapies such as checkpoint inhibitors (ICI), the immune response against cancer cells can be reactivated.
Second Opinion
An opinion of a doctor other than the patient’s current doctor.
A second opinion is when a patient seeks the advice of another doctor or healthcare specialist unrelated to the first opinion to review their diagnosis, and treatment options. The second-opinion doctor reviews the patient’s medical records and provides a diagnosis and treatment pathway based on their professional opinion. Seeking a second opinion can provide the patient with additional information, peace of mind, and assurance that they are receiving the best possible care. It can also help the patient to make informed decisions about their health and treatment options.
A second opinion is when a patient seeks the advice of another doctor or healthcare specialist unrelated to the first opinion to review their diagnosis, and treatment options. The second-opinion doctor reviews the patient’s medical records and provides a diagnosis and treatment pathway based on their professional opinion. Seeking a second opinion can provide the patient with additional information, peace of mind, and assurance that they are receiving the best possible care. It can also help the patient to make informed decisions about their health and treatment options.
Note: Second Opinions from doctors who have proven current expertise and experience with cholangiocarcinoma have been a hallmark in achieving improved and successful patient outcomes
TMB
Tumor Mutational Burden.
TMB refers to the total number of mutations in a tumor’s DNA, and high TMB has been associated with a higher likelihood of response to immunotherapy treatments such as checkpoint inhibitors. TMB has been studied in a variety of cancer types, including cholangiocarcinoma, and has shown promising results as a biomarker for predicting response to immunotherapy.
Tumor
Tumors are a mass of tissue that’s formed by an accumulation of abnormal cells. Normally, the cells in your body age, die and are replaced by new cells. With cancer and other tumors, something disrupts this cycle.
Tumor – Primary
A primary tumor is the original tumor that develops in a specific location in the body. It can be benign or malignant, and if it is malignant, it has the potential to spread to other parts of the body, forming secondary tumors.
TMN (Staging)
TMN is a scoring system to grade and stage the extent and spread of a cancerous tumour.
The letters T, N, and M stand for Tumor, Node, and Metastasis, respectively.
- The T category describes the size and extent of the primary tumor,
- The N category describes the involvement of nearby lymph nodes, and
- The M category describes whether or not the cancer has spread to distant organs or tissues.
- Each category is assigned a number or letter (usually from 0 to 4) to further describe the extent and severity of the cancer.
- The TMN score is used by your doctor to determine the stage of the cancer, which can help guide treatment decisions and predict a prognosis.
Coming Soon
Apologies for the delay
come back soon
What are MSi-high /dMMR Cancers
HOW A TEST FOR MSI‑H/dMMR WORKS
Important View Immuno 101
Everyone’s cancer is different. To help develop a treatment plan that’s right for you, your doctor may order laboratory tests. These tests can evaluate your tumor for different biomarkers, including MSI‑H or dMMR. Some biomarkers are used to help select patients that may benefit from certain treatments, such as KEYTRUDA. Talk to your doctor to see if a laboratory test for the MSI‑H or dMMR biomarker is right for you.
- A tissue sample (biopsy) of your tumor is taken, and your doctor orders the test.
- Your doctor typically gets the results in 10 to 14 days.
- You talk with your doctor to discuss treatment options based on your results.
- You may begin treatment with KEYTRUDA if you and your doctor have decided it’s right for you.
Clinical Trial Websites
Testing the tissue of a tumour
IHC – Immunohistochemical or
Genomic Profiling / Molecular Profiling
Both these tests will highlight PD-L1, MSi Status, MMR and HER2
- IHC: Fast 3-5 day turnaround versus Molecular Profiling (4-6 weeks) This allows for quicker treatment response.
- IHC and Molecular Profiling results agree 92% of the time
- IHC is inexpensive versus Molecular Profiling
- Genomic Profiling should be immediately ordered if an IHC test is unsuccessful.
- Genomic Profiling is able to look at the whole tumour environment and mostly discover the mutation type that is driving the mutation and the cancers growth.
What are PD-1 and PD-L1 biomarkers
CANCER CELLS MAY USE THE PD-1 PATHWAY TO HIDE FROM T CELLS
Important View Immuno 101
The immune system is your body’s natural defense against disease. The immune system sends certain types of cells called T cells throughout your body to detect and fight infections and diseases—including cancer.
Cancer cells may use the PD-1 pathway to hide from T cells. This stops T cells from attacking cancer cells and allowing cancer cells to grow and spread.
PD‑1 = programmed death receptor-1
PD-1 and PD-L1 are types of proteins found on cells in your body. PD‑1 protein is found on immune cells called T cells. It normally acts as a type of “off switch” that helps keep the T cells from attacking other cells in the body. PD-1 attaches to PD‑L1, a protein found on some normal (and cancer) cells. This interaction basically tells the T cell to leave the other cell alone and not attack it. Some cancer cells have large amounts of PD‑L1, which helps them hide from immune attack.
Therapies that target either PD-1 or PD-L1 can stop them from attaching and help keep cancer cells from hiding.
Learn more about KEYTRUDA, a type of immunotherapy that works by blocking the PD‑1 pathway.
KEYTRUDA can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. These problems may happen anytime during treatment or even after your treatment has ended.
Information Source: https://www.keytruda.com/how-does-keytruda-work/