Cholangio 101
CHOLANGIOCARCINOMA (CCA)
Cancer within the bile duct, thereafter the primary location of origin further defines the subtype of your specific Cholangiocarcinoma diagnosis.
Pronunciation
Cholangiocarcinoma is the clinical name for Bile Duct Cancer.
The easiest way to pronounce this name is to first break it in half, ie: Cholangio + carcinoma
Chol – angio + car – cinoma
Listen to the pronunciation
Meaning
- Chol’e means bile +
- angio means vessel – ie Bile Duct tube +
- carcinoma means a type of cancer that grows in the tissue lining the body’s organs
Cholangiocarcinoma is cancer that begins in the bile ducts.
Cholangiocarcinoma is the clinical name for bile duct carcinoma.
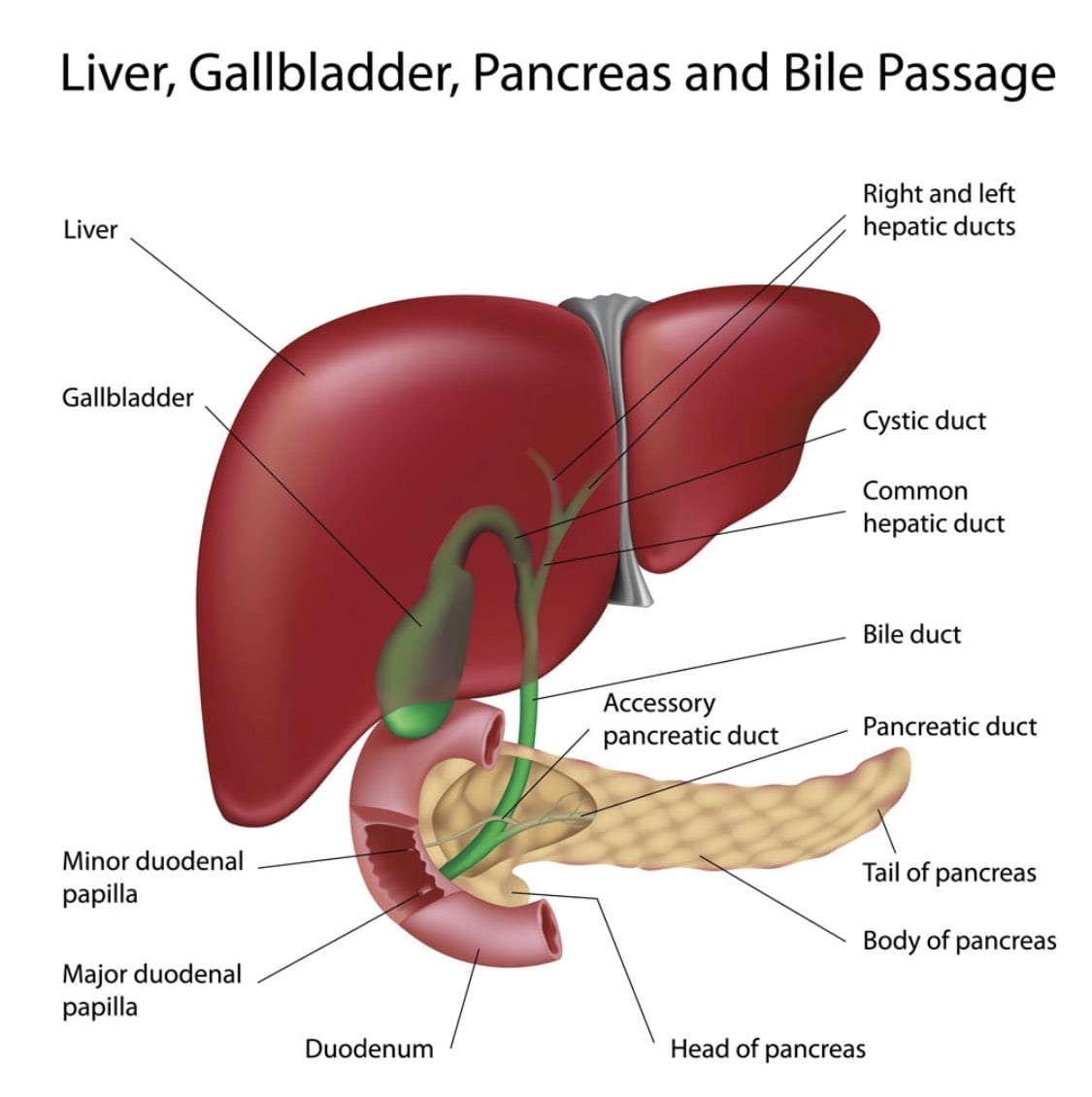
The bile duct system is like a network of bile streams called ductules originating in the liver and then feeding down to form two larger ducts. Think of two networks of streams coming together – a right network and a left network.
These two ducts are called the “Left” and “Right” “Hepatic Ducts” which join together and form one common bile duct. This area is referred to as the “Hilar region” or more recently the “Perihilar” region. (Hilar means slit or opening)
The “Common bile duct” tube is about 125 -150 mm long, extending from the liver to the small intestine called the Duodenum. The bile duct’s function is to move a fluid called bile from the liver and gallbladder to the small intestine, where it helps digest the fats in food.
About one-third of the way down the common bile duct, the gallbladder (an organ that stores bile) attaches by a small duct called the cystic duct.
The common bile duct then passes down through part of the pancreas before it empties into the first part of the small intestine (the duodenum), next to where the pancreatic duct also enters the small Duodenum.
Primary Tumours
(Means location where the cancer begins)
Primary Tumours can develop in any part of the bile duct and are named after their exact location –
Click each type below to see more
- iCCA: Intrahepatic cholangiocarcinoma
- pCCA: Perihilar cholangiocarcinoma
- dCCA: Distal cholangiocarcinoma
Intrahepatic Cholangiocarcinoma
Intrahepatic CCA occurs inside the liver where cancer develops in the hepatic bile ducts or the smaller intrahepatic biliary ducts. In some cases, patients express a combined diagnosis.
Perihilar (Hilar or Klatskin Tumor) Cholangiocarcinoma
These cancers develop where the right and left hepatic ducts have joined and are leaving the liver. These are the most common type of cholangiocarcinoma accounting for more than half of all bile duct cancers.
Distal Cholangiocarcinoma
Distal CCA occurs outside the liver after the right and left hepatic bile ducts have joined to form the common bile duct. This type of cancer is found where the common bile duct passes through the pancreas and into the small intestine.
Extrahepatic Cholangiocarcinoma
Because perihilar and distal bile duct cancers start outside the liver, they are often grouped together and referred to as extrahepatic cholangiocarcinoma.
Cholangiocarcinoma can also be divided into types based on how the cancer cells look under the microscope.
More than 95% of bile duct cancers are carcinomas and most are adenocarcinomas.
Adenocarcinomas are cancer that begins in the glandular (secretory) cells. Glandular cells are found in epithelial tissue (Skin layer) that lines and protects internal organs. These glandular cells make and release substances such as mucus, digestive juices, or other fluids to protect the skin layer.
Symptoms most often appear late ie stage 3 – 4
Sudden onset of abdominal pain, Fatigue, then jaundice, and weight loss. These symptoms are similar to many other ailments in the beginning and therefore often dismissed.
There is no current early detection method for Cholangiocarcinoma.
It is unfortunate that most patients will feel no ill effects until the cancer is very advanced. This is one of Cholangiocarcinoma’s biggest threats, and contributes to many being excluded from potentially curative surgery.
Most Common Symptoms
- Chills
- Clay-colored stools
- Fever
- Itching
- Loss of appetite
- Weight loss
- Pain in the upper right abdomen that may radiate to the back
- Yellowing of the skin
The video below discusses the onset of symptoms.
Although this video is focused on the ‘Hilar’ it is essentially the same symptoms for all cholangiocarcinoma tumour locations.
Intrahepatic Cholangiocarcinoma:
A network of tubes, called ducts, connects the liver, gallbladder, and small intestine. This network begins in the liver where many small ducts collect bile (a fluid made by the liver to break down fats during digestion). The small ducts come together to form the right and left hepatic ducts, which lead out of the liver. The two ducts join outside the liver and form the common hepatic duct. The cystic duct connects the gallbladder to the common hepatic duct. Bile from the liver passes through the hepatic ducts, common hepatic duct, and cystic duct and is stored in the gallbladder.
When food is being digested, bile stored in the gallbladder is released and passes through the cystic duct to the common bile duct and into the small intestine.
Bile duct cancer is also called cholangiocarcinoma.
There are two primary types of bile duct cancer:
Intrahepatic Cholangiocarcinoma:
This type of cancer forms in the bile ducts inside the liver. Only a small number of bile duct cancers are intrahepatic. Intrahepatic bile duct cancers are also called intrahepatic cholangiocarcinomas.
CLICK IMAGE TO ENLARGE
Anatomy of the intrahepatic bile ducts.
Intrahepatic bile ducts are a network of small tubes that carry bile inside the liver. The smallest ducts, called ductules, come together to form the right hepatic bile duct and the left hepatic bile duct, which drain bile from the liver. Bile is stored in the gallbladder and is released when food is being digested.
Extrahepatic Cholangiocarcinoma:
This type of cancer forms in the bile ducts outside the liver. The extrahepatic bile duct is made up of the hilum region and the distal region. Cancer can form in either region:
Perihilar:
This type of cancer is found in the hilum region, the area where the right and left bile ducts exit the liver and join to form the common hepatic duct. Perihilar bile duct cancer is also called a Klatskin tumor or perihilar cholangiocarcinoma.
Distal:
This type of cancer is found in the distal region. The distal region is made up of the common bile duct which passes through the pancreas and ends in the small intestine. Distal bile duct cancer is also called extrahepatic cholangiocarcinoma.
CLICK TO ENLARGE IMAGE
Anatomy of the extrahepatic bile ducts.
Extrahepatic bile ducts are small tubes that carry bile outside of the liver. They are made up of the common hepatic duct (hilum region) and the common bile duct (distal region). Bile is made in the liver and flows through the common hepatic duct and the cystic duct to the gallbladder, where it is stored. Bile is released from the gallbladder when food is being digested.
Stages of Cholangiocarcinoma
KEY POINTS
- The results of diagnostic and staging tests are used to find out if cancer cells have spread.
- There are three ways that cancer spreads in the body.
- Cancer may spread from where it began to other parts of the body.
- Stages are used to describe the different types of bile duct cancer.
- Intrahepatic Cholangiocarcinoma
- Perihilar Cholangiocarcinoma
- Distal Cholangiocarcinoma
The following groups are used to plan treatment:
- Resectable (localised) bile duct cancer
- Unresectable (including metastatic and recurrent) bile duct cancer
Stages are used to describe the different types of Cholangiocarcinoma
Intrahepatic Cholangiocarcinoma
Stage 0: In stage 0 intrahepatic bile duct cancer, abnormal cells are found in the innermost layer of tissue lining the intrahepatic bile duct. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
Stage I: Stage I intrahepatic bile duct cancer is divided into stages IA and IB.
CLICK IMAGE TO ENLARGE
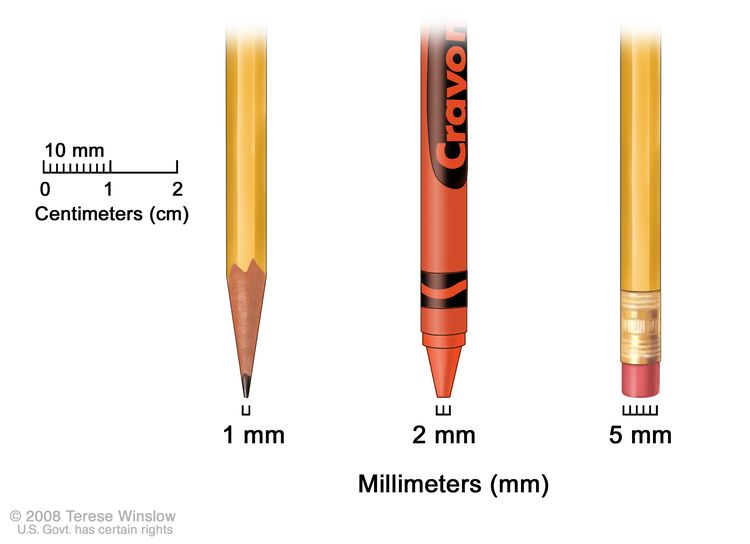
Tumor sizes are often measured in centimeters (cm) or inches. Common food items that can be used to show tumor size in cm include: a pea (1 cm), a peanut (2 cm), a grape (3 cm), a walnut (4 cm), a lime (5 cm or 2 inches), an egg (6 cm), a peach (7 cm), and a grapefruit (10 cm or 4 inches).
- In stage IA, cancer has formed in an intrahepatic bile duct and the tumor is 5 centimeters or smaller.
- In stage IB, cancer has formed in an intrahepatic bile duct and the tumor is larger than 5 centimeters.
Stage II: In stage II intrahepatic bile duct cancer, either of the following is found:
- the tumor has spread through the wall of an intrahepatic bile duct and into a blood vessel; or
- more than one tumor has formed in the intrahepatic bile duct and may have spread into a blood vessel.
Stage III: Stage III intrahepatic bile duct cancer is divided into stages IIIA and IIIB.
- In stage IIIA, the tumor has spread through the capsule (outer lining) of the liver.
- In stage IIIB, cancer has spread to organs or tissues near the liver, such as the duodenum, colon, stomach, common bile duct, abdominal wall, diaphragm, or the part of the vena cava behind the liver, or the cancer has spread to nearby lymph nodes.
Stage IV: In stage IV intrahepatic bile duct cancer, cancer has spread to other parts of the body, such as the bone, lungs, distant lymph nodes, or tissue lining the wall of the abdomen and most organs in the abdomen.
Perihilar bile duct cancer
Stage 0: In stage 0 perihilar bile duct cancer, abnormal cells are found in the innermost layer of tissue lining the perihilar bile duct. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ or high-grade dysplasia.
Stage I: In stage I perihilar bile duct cancer, cancer has formed in the innermost layer of tissue lining the perihilar bile duct and has spread into the muscle layer or fibrous tissue layer of the perihilar bile duct wall.
Stage II: In stage II perihilar bile duct cancer, cancer has spread through the wall of the perihilar bile duct to nearby fatty tissue or to liver tissue.
Stage III: Stage III perihilar bile duct cancer is divided into stages IIIA, IIIB, and IIIC.
- Stage IIIA: cancer has spread to branches on one side of the hepatic artery or of the portal vein.
- Stage IIIB: cancer has spread to one or more of the following:
– the main part of the portal vein or its branches on both sides;
– the common hepatic artery;
– the right hepatic duct and the left branch of the hepatic artery or of the portal vein;
– the left hepatic duct and the right branch of the hepatic artery or of the portal vein. - Stage IIIC: cancer has spread to 1 to 3 nearby lymph nodes.
Stage IV: Stage IV perihilar bile duct cancer is divided into stages IVA and IVB.
- Stage IVA: Cancer has spread to 4 or more nearby lymph nodes.
- Stage IVB: Cancer has spread to other parts of the body, such as the liver, lung, bone, brain, skin, distant lymph nodes, or tissue lining the wall of the abdomen and most organs in the abdomen.
Distal bile duct cancer
Stage 0: In stage 0 distal bile duct cancer, abnormal cells are found in the innermost layer of tissue lining the distal bile duct. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ or high-grade dysplasia.
Millimeters (mm). A sharp pencil point is about 1 mm, a new crayon point is about 2 mm, and a new pencil eraser is about 5 mm.
Stage I: In stage I distal bile duct cancer, cancer has formed and spread fewer than 5 millimeters into the wall of the distal bile duct.
Stage II: Stage II distal bile duct cancer is divided into stages IIA and IIB.
- Stage IIA: Cancer has spread:
– fewer than 5 millimeters into the wall of the distal bile duct and has spread to 1 to 3 nearby lymph nodes; or
– 5 to 12 millimeters into the wall of the distal bile duct. - Stage IIB: Cancer has spread 5 millimeters or more into the wall of the distal bile duct. Cancer may have spread to 1 to 3 nearby lymph nodes.
Stage III: Stage III distal bile duct cancer is divided into stages IIIA and IIIB.
- Stage IIIA: Cancer has spread into the wall of the distal bile duct and to 4 or more nearby lymph nodes.
- Stage IIIB: Cancer has spread to the large vessels that carry blood to the organs in the abdomen. Cancer may have spread to 1 or more nearby lymph nodes.
Stage IV: In stage IV distal bile duct cancer, cancer has spread to other parts of the body, such as the liver, lungs, or tissue lining the wall of the abdomen and most organs in the abdomen.
First-line Treatment
Firstline treatment means the medically accepted and practiced first approach. If unsuccessful a second-line approach will be looked at…etc. For more information on treatments please visit our Treatments 101
Key Points
Please note: This information is derived from the USA National Cancer Center and should be used as a guideline only
- There are different types of treatment for patients with bile duct cancer.
- Three types of standard treatment are used:
– Surgery
– Radiation therapy
– Chemotherapy - New types of treatment are being tested in clinical trials.
– Liver transplant
– Targeted therapy
– Immunotherapy - Treatment for bile duct cancer may cause side effects.
- Patients may want to think about taking part in a clinical trial.
- Patients can enter clinical trials before, during, or after starting their cancer treatment.
- Follow-up tests may be needed.
Side-effects of treatment
Side effects vary greatly and will depend on the specific type of treatment you are receiving. Treating physicians and clinical trials will discuss this before you proceed.
There are different types of treatment for patients with Cholangiocarcinoma
Different types of treatments are available for patients with bile duct cancer. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Three types of standard treatment are used:
Surgery
The following types of surgery are used to treat bile duct cancer:
- Removal of the bile duct: A surgical procedure to remove part of the bile duct if the tumor is small and in the bile duct only. Lymph nodes are removed and tissue from the lymph nodes is viewed under a microscope to see if there is cancer.
- Partial hepatectomy: A surgical procedure in which the part of the liver where cancer is found is removed. The part removed maybe a wedge of tissue, an entire lobe, or a larger part of the liver, along with some normal tissue around it.
- Whipple procedure: A surgical procedure in which the head of the pancreas, the gallbladder, part of the stomach, part of the small intestine, and the bile duct are removed. Enough of the pancreas is left to make digestive juices and insulin.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
External and internal radiation therapy is used to treat bile duct cancer.
It is not yet known whether external radiation therapy helps in the treatment of resectable bile duct cancer. In unresectable, metastatic, or recurrent bile duct cancer, new ways to improve the effect of external radiation therapy on cancer cells are being studied:
- Hyperthermia therapy: A treatment in which body tissue is exposed to high temperatures to make cancer cells more sensitive to the effects of radiation therapy and certain anticancer drugs.
- Radiosensitizers: Drugs that make cancer cells more sensitive to radiation therapy. Combining radiation therapy with radiosensitizers may kill more cancer cells.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
Systemic chemotherapy is used to treat unresectable, metastatic, or recurrent bile duct cancer. It is not yet known whether systemic chemotherapy helps in the treatment of resectable bile duct cancer.
In unresectable, metastatic, or recurrent bile duct cancer, intra-arterial embolization is being studied. It is a procedure in which the blood supply to a tumor is blocked after anticancer drugs are given in blood vessels near the tumor. Sometimes, the anticancer drugs are attached to small beads that are injected into an artery that feeds the tumor. The beads block blood flow to the tumor as they release the drug. This allows a higher amount of drug to reach the tumor for a longer period of time, which may kill more cancer cells.
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI website. This is USA specific – but will give you an overview
Liver transplant
In a liver transplant, the entire liver is removed and replaced with a healthy donated liver. A liver transplant may be done in patients with perihilar bile duct cancer. If the patient has to wait for a donated liver, other treatment is given as needed.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do. The following targeted therapies are being studied in patients with bile duct cancer that is locally advanced and cannot be removed by surgery or has spread to other parts of the body:
- Ivosidenib is a type of targeted therapy that blocks a specific mutation in a gene called IDH1. It works by slowing or stopping the growth of cancer cells.
- Pemigatinib and infigratinib are types of targeted therapies that block specific changes in a gene called FGFR2. This may help keep cancer cells from growing and may kill them.
Immunotherapy
Immunotherapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This cancer treatment is a type of biologic therapy.
Immune checkpoint inhibitor therapy is a type of immunotherapy that may be used to treat bile duct cancer.
- PD-1 and PD-L1 inhibitor therapy: PD-1 is a protein on the surface of T cells that helps keep the body’s immune responses in check. PD-L1 is a protein found on some types of cancer cells. When PD-1 attaches to PD-L1, it stops the T cell from killing the cancer cell. PD-1 and PD-L1 inhibitors keep PD-1 and PD-L1 proteins from attaching to each other. This allows the T cells to kill cancer cells. Pembrolizumab is a type of PD-1 inhibitor that may be used in patients whose cancer is locally advanced and cannot be removed by surgery or has spread to other parts of the body.
Immune checkpoint inhibitor. Checkpoint proteins, such as PD-L1 on tumor cells and PD-1 on T cells, help keep immune responses in check. The binding of PD-L1 to PD-1 keeps T cells from killing tumor cells in the body (left panel). Blocking the binding of PD-L1 to PD-1 with an immune checkpoint inhibitor (anti-PD-L1 or anti-PD-1) allows the T cells to kill tumor cells (right panel).
Immunotherapy uses the body’s immune system to fight cancer. This animation explains one type of immunotherapy that uses immune checkpoint inhibitors to treat cancer.
Treatment for bile duct cancer may cause side effects.
For information about side effects caused by treatment for cancer, see Side Effects page. (USA)
You may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
You can enter clinical trials before, during, or after starting their cancer treatment.
This is USA content but it is accurate and will provide an overview
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment of Resectable (Localized) Bile Duct Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of resectable intrahepatic bile duct cancer may include:
- Surgery to remove the cancer, which may include partial hepatectomy. Embolization may be done before surgery.
Treatment of resectable perihilar bile duct cancer many include:
- Surgery to remove the cancer, which may include partial hepatectomy.
- Stent placement or percutaneous transhepatic biliary drainage as palliative therapy, to relieve jaundice and other symptoms and improve the quality of life.
Treatment of resectable distal bile duct cancer may include:
- Surgery to remove the cancer, which may include a Whipple procedure.
- Stent placement or percutaneous transhepatic biliary drainage as palliative therapy, to relieve jaundice and other symptoms and improve the quality of life.
Adjuvant therapy for resectable bile duct cancer may include:
- Chemotherapy.
- External-beam radiation therapy.
- A clinical trial of adjuvant therapy.
Use the (USA) clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Unresectable Bile Duct Cancer (Including Metastatic or Recurrent Disease)
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of unresectable bile duct cancer (including metastatic or recurrent disease) may include:
- Stent placement or biliary bypass as palliative treatment to relieve symptoms and improve the quality of life.
- External or internal radiation therapy as palliative treatment to relieve symptoms and improve the quality of life.
- Combination chemotherapy.
- A clinical trial of various combinations of chemotherapy.
- A clinical trial of immunotherapy in patients with mutations (changes) in certain genes.
- A clinical trial of targeted therapy in patients with mutations (changes) in certain genes.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Good resources for terminologies
What is Primary Cancer?
This is the original tumour location. A tumour in the bile duct is called a Cholangiocarcinoma if it spreads (Metastasises) to other parts of the body ie. Lungs, it is still Cholangiocarcinoma, not lung cancer, etc.
What is Metastasis?
When the cancer spreads to other locations away from its primary tumour location ie. Lungs, Liver, etc.
What is a Mutation?
Any change in the DNA sequence of a cell. Mutations may be caused by mistakes during cell division, or they may be caused by exposure to DNA-damaging agents in the environment.
What are the Curative Options?
- Surgical operations are the only known Curative action, but stats are very poor
- More recently immunotherapy has been seen as a curative option
What are the Surgery Procedures?
- ECRP: Surgical, typically investigative same-day procedure via the mouth
- Whipple: Surgical, a significant operation typically removing all or part of multiple sites such as gallbladder, head of the pancreas, and stomach
- Resection: Surgical, typically refers to Intrahepatic patients, removing a portion of the liver and gallbladder. This can also refer to removing a section of the bile duct for Extrahepatic patients which often include the gallbladder.
What is Chemotherapy?
- A drug that is infused or oral
- Typically the first line action is Gem/Cis – Gemcitabine & Cisplatin
- Chemotherapy is not regarded as curative, but the best management tool available
- Chemotherapy is an infusion process carried out in the Chemo wards of most hospitals, typically this will take 3 – 5 hours. Some Chemotherapy options such as Capecitabine are taken orally
Most treatment programs are 3 to 6 months in length and can be repeated several times.
What is the CA 19- 9 Marker?
A measure in a blood test (carbohydrate antigen) – a tumor marker that is observed in elevated serum concentration with metastatic GI cancers. This is not always an accurate measurement.
What are Clinical Trials?
There are many trials coming available in both immunotherapy and combination immunotherapy and Chemotherapy. Most patients embrace trials as an opportunity to move forward.
What is Immunology?
Immunology is a fast-evolving knowledge pool of using the body’s immune system to defeat cancer. Immunotherapy is the specifically designed option derived from the immunology pool that is applied to the patient. This is worth reading up about …[continue]
About; Adenocarcinoma, Carcinoma & Epithelial tissue
Adenocarcinoma may occur almost anywhere in the body, starting in glands that line the insides of the organs. Adenocarcinoma forms in glandular epithelial cells, which secrete mucus, digestive juices, or other fluids.
Adenocarcinomas are a subtype of carcinoma, the most common form of cancer, and typically forms solid tumors.
Carcinomas are the most common type of cancer. they begin in the epithelial tissue of the skin, or in the tissue that lines internal organs, such as the liver or kidneys. Carcinomas may spread to other parts of the body, or be confined to the primary location.
Carcinomas can occur in any of these organs. Common types include breast cancer, colorectal cancer, lung cancer, pancreatic cancer, and prostate cancer.
Epithelial tissues are widespread throughout the body. They form the covering of all body surfaces, line body cavities and hollow organs, and are the major tissue in glands. They perform a variety of functions that include protection, secretion, absorption, excretion, filtration, diffusion, and sensory reception.
Intrahepatic
Intrahepatic bile ducts are a network of small tubes that carry bile inside the liver. The smallest ducts, called ductules, come together to form the right hepatic bile duct and the left hepatic bile duct, which drain bile from the liver. Bile is stored in the gallbladder and is released when food is being digested.

Perihilar
Perihiar is a subtype of Extrahepatic Cholangiocarcinoma
A small part of a duct (tube) called the extrahepatic bile duct that is just outside the liver and carries bile from the liver and gallbladder to the small intestine. The perihilar bile duct starts where the right and left hepatic ducts join outside the liver and form the common hepatic duct.
- Often also referred to as Hilar or Klastskin tumours and
- Hilum region.
Distal
Distal is a subtype of Extrahepatic Cholangiocarcinoma
Distal bile duct cancer: This type of cancer is found in the distal region. The distal region is made up of the common bile duct which passes through the pancreas and ends in the small intestine. Distal bile duct cancer is also called extrahepatic cholangiocarcinoma.